- 1058
- 6.7 Minute
Pneumonia: A Silent Lung Infection That Demands Early Action
Pneumonia remains a major public-health concern, affecting people across all age groups and placing a heavy burden on families and the healthcare system. In my daily practice, I meet many patients, from small children to the elderly, who arrive with sudden breathing difficulty, high fever, and weakness caused by this infection. The disease not only disrupts personal and professional life but, when ignored, can escalate into severe complications needing hospital or ICU care.
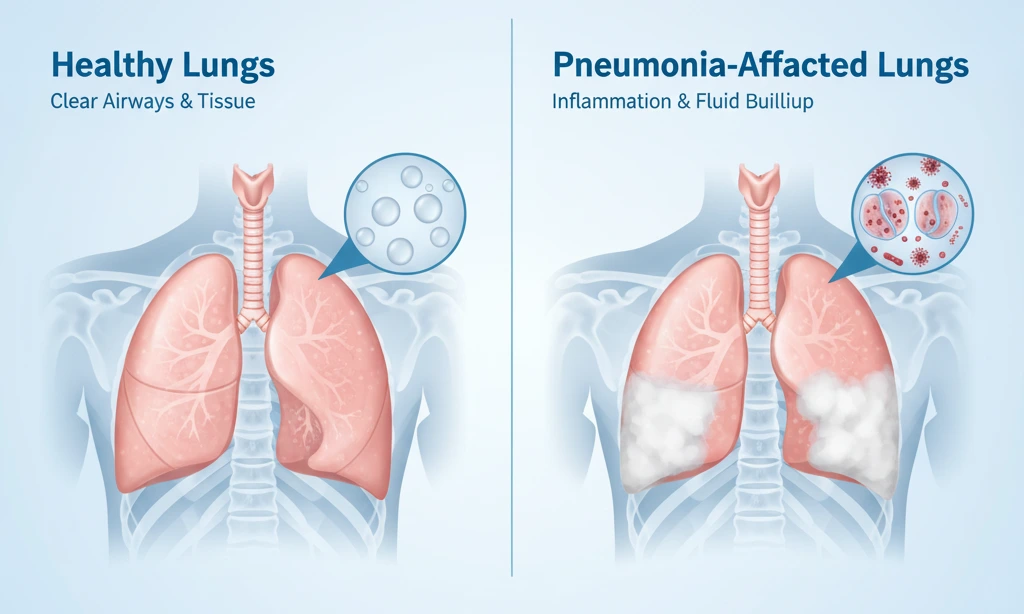
In simple terms, pneumonia is a condition in which the lungs become infected and the tiny air sacs (alveoli) fill with fluid or pus. This blocks normal airflow, reduces oxygen supply to the body, and makes breathing painful and difficult. Although some patients experience a mild form, others—especially high-risk individuals—can develop a dangerous, rapidly worsening illness.
The illness usually begins with symptoms such as fever, chills, cough, chest tightness, and breathlessness. Patients may feel extremely tired, lose appetite, or in the case of older adults, show signs of confusion or disorientation. These warning signs should never be ignored.
Pneumonia develops due to several causes—bacteria remain the most common culprits, but viruses (including influenza and COVID-19) and fungi can also lead to infection. In elderly or bedridden patients, food or liquids entering the lungs can trigger aspiration pneumonia.
To confirm pneumonia, doctors rely on a combination of clinical examination and investigations like chest X-ray, blood tests, sputum culture, and oxygen saturation monitoring. In complicated situations or when symptoms do not match the X-ray, a CT scan may be required for clarity.

Treatment varies based on the cause. Bacterial pneumonia usually improves with timely antibiotics. Viral pneumonia requires supportive care along with suitable antiviral medication. Rest, adequate fluid intake, fever control, and oxygen support, when necessary, form the backbone of management. Severe cases may need ventilator support.
If not treated early, pneumonia can progress to complications such as fluid accumulation around the lungs (pleural effusion), formation of a lung abscess, respiratory failure, or life-threatening sepsis. These conditions demand immediate and aggressive treatment, often in a hospital setting.
Hospital admission is especially important when patients have low oxygen levels, extremely fast breathing, high fever, low blood pressure, altered mental status, or severe findings on chest imaging. Individuals with diabetes, heart disease, COPD, asthma, or low immunity also need close monitoring.
The risk of pneumonia is higher in children under five, older adults above sixty-five, smokers, chronic alcohol users, diabetics, people with lung or heart diseases, those living in polluted environments, and individuals with weakened immune systems.
Despite its seriousness, pneumonia is preventable. Regular handwashing, avoiding smoking, maintaining a balanced lifestyle, staying physically active, and following vaccination schedules play a vital role. The pneumococcal vaccine, annual influenza shot, and recommended COVID-19 boosters offer strong protection, especially for vulnerable groups.

As a pulmonologist, I strongly encourage everyone to stay alert to the early signs of pneumonia and seek medical care without delay. With proper awareness, preventive measures, and timely treatment, we can greatly reduce the impact of this potentially dangerous lung infection on individuals and society.
Frequently Asked Questions
Pneumonia is a lung infection in which the air sacs (alveoli) fill with fluid or pus, making it difficult for oxygen to reach the bloodstream. It can be caused by bacteria, viruses, or fungi.
Common symptoms include fever, cough, chills, chest pain, breathing difficulty, fatigue, and loss of appetite. Older adults may also show confusion or sudden weakness.
Yes. Many types—especially bacterial and viral pneumonias—can spread from person to person through coughing, sneezing, or close contact. Aspiration pneumonia, however, is not contagious.
Children under 5, adults over 65, smokers, diabetics, patients with asthma or COPD, bedridden individuals, and people with weakened immunity are at higher risk.
Doctors use physical examination, chest X-rays, blood tests, sputum culture, oxygen saturation checks, and sometimes CT scans when needed.
Treatment depends on the cause—antibiotics for bacterial pneumonia, antiviral medications for viral infections, and antifungal drugs when fungi are involved. Supportive care such as fluids, rest, fever control, and oxygen therapy may also be required.
Hospitalization is needed for severe pneumonia, low oxygen levels, very high fever, low blood pressure, rapid breathing, confusion, or complications. High-risk patients should be monitored closely.